Difference between revisions of "From Fructose to Alzheimer's"
(→Traumatic Brain Injury (TBI): deleted prompt to insert graphic) |
|||
| Line 117: | Line 117: | ||
== This is still a hypothesis == | == This is still a hypothesis == | ||
While the similarities between fructose and Alzheimer's are | While the similarities between fructose and Alzheimer's are compelling, the science is not settled and there are some issues that need to be better understood. Further studies are needed. Also, tThe intricacies of this hypothesis are also far more involved than what has been represented here, this wiki endeavored to provide the most salient points of this hypothesis. | ||
== About the lead researcher, Richard J. Johnson == | == About the lead researcher, Richard J. Johnson == | ||
Revision as of 10:13, 10 March 2023
UNDER CONSTRUCTION
Fructose is a sugar that produces unique physiological effects.
Fructose decreases production of cellular ATP (adenosine triphosphate). ATP is produced by the mitochondria to provide energy for cells, see Mitochondria. This lowered energy triggers a desire to eat more. Chronic fructose consumption induces leptin resistance. Leptin is the satiety hormone that helps maintain a healthy weight, but leptin resistance dulls that feeling of satiety, also increasing susceptibility for overeating. Fructose is turned into uric acid which can cause kidney stones, gout, and high blood pressure. Studies show that high fructose increases the risk of non-alcoholic fatty liver disease (NAFLD). Fructose increases triglycerides and increases LDL (the “bad” cholesterol). Fructose leads to health problems such as obesity and Type 2 Diabetes. And recently, (2023) a hypothesis has been revealed that fructose is a major contributor to Alzheimer’s Disease.
So why is fructose so “mean” to us? Actually, it doesn’t seem to be the fructose, but rather modern diet. Fructose’s unique physiological effects are meant to aid in survival during times of scarcity, which man faced with regularity during most of human existence.

While fructose can be consumed from natural and processed food sources, under certain circumstances, which the body perceives as times of scarcity, the body can produce its own (endogenous) fructose, even without consuming fructose. The non-fructose dietary drivers of endogenous fructose production are prevalent in the modern western diet. So what was once a survival mechanism for ancient man appears to be what is playing a role in developing Alzheimer’s and other chronic diseases for modern man.
Granted, the causes of Alzheimer’s are not fully understood, and this paper Could Alzheimer’s disease be a maladaptation of an evolutionary survival pathway mediated by intracerebral fructose and uric acid metabolism?(Richard J. Johnson et al, Mar 2023) offers another hypothesis to add to the pile. But this new hypothesis interleaves very well with many established research findings on Alzheimer’s, including reduced cerebral glucose metabolism, mitochondrial dysfunction, neuroinflammation, and intracellular energy depletion. It also aligns with the Bredesen Protocol, see Bredesen Protocol. In fact, Dr Dale Bredesen is one of the co-authors of this paper, as is Neurologist Dr David Perlmutter, author of Grain Brain and other NY Times best seller books. So for those who follow Dr Bredesen’s protocol, no changes are necessary, it already keeps fructose pathway activation minimized. But these findings do add greater weight to following Dr Bredesen's protocol if trying to prevent Alzheimer’s.
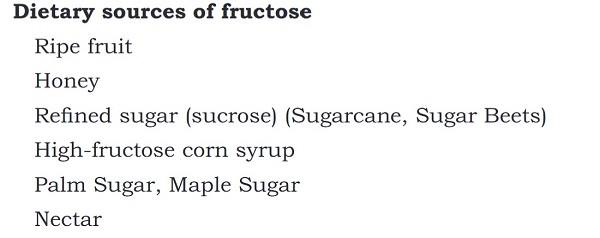
Introduction to sugar

When we think of sugar, we commonly think of table sugar. Table sugar is sucrose, a refined from sugar cane or sugar beets. It contains both glucose and fructose.
Glucose is the body’s primary fuel, sometimes called blood sugar. see Blood Sugar. Glucose can be used by every cell in the body, but too much glucose is stored as fat on the body. Glucose is especially important for the brain. While constituting only 3% of the body's mass, the brain uses approximately 20% of the body's energy and it needs that energy source 24 hours a day to sustain neurons and function optimally. see Insulin Resistance in the Brain. The brain’s energy needs can be aided by ketones, but there are some cells in the brain that can only burn glucose. Carbohydrates are a common dietary source for the body to turn into glucose, although, because glucose is an imperative for the brain and muscles, the body can also make glucose from non-carbohydrate precursors (triglycerides, lactate, protein) via a process called gluconeogenesis. Do note that simply consuming carbohydrates doesn’t assure glucose for the brain to access.
High fructose corn syrup (HFCS) is a refined sugar added to many processed foods, even ones that aren’t sweet such as sauces, condiments, salad dressing, 12 Common Foods with High Fructose Corn Syrup. HFCS consists of both glucose and fructose and is sweeter than table sugar.
Fructose is a sugar found naturally in fruit and honey. But fructose is also made in the body, a major discussion point of this wiki article. Regardless of source: natural sources (fruit, honey), refined sources (sucrose, high fructose corn syrup), or made endogenously (by the body) the effects of excess fructose are the same.
Survival Pathway Triggered by Fructose
Food is more than calories, food also provides “information” for the body. In nature, animals use excessive intake and metabolism of fructose to activate a survival response that prepares them for periods when food, water, or oxygen may not be adequately available.

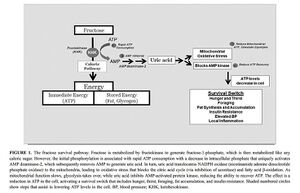
From Fructose metabolism as a common evolutionary pathway of survival associated with climate change, food shortage and droughts (R. J. Johnson et al, 17 October 2019)
- Specifically, fructose shifts the energy provided in nutrients towards fuel storage (fat, glycogen) and away from energy (ATP) production by downregulating mitochondrial metabolism and the favouring of glycolysis. The fat and glycogen provide a source forenergy and metabolic water when food and water are scarce. The switch towards glycolysis is associated with a reduction in energy demand and results in protection from hypoxic and ischaemic states. Gluconeogenesis and insulin resistance occur to raise serum glucose levels to provide fuel to the brain. Sodium is retained, and vasoconstrictors are stimulated to increase blood pressure, and innate immunity is also stimulated. Foraging develops, and thirst and hunger occur as a mechanism to increase weight, largely from the development of leptin resistance and hyperosmolality-driven thirst. These processes are mediated by end products of fructose metabolism that include vasopressin, lactate and uric acid. While providing a key survival advantage in conditions of scarce resources, excessive fructose can stimulate metabolic diseases, dementia and cancer.
Effects of Fructose on the brain
The brain is an energy hog. In comparison to other organs of the body, the brain needs a disproportionate supply of energy and it needs this energy 24 hours a day, every day. The high energy needs of neurons are accomplished by mitochondrial oxidative phosphorylation of glucose, which requires sufficient oxygen to be present.
Neurons prefer glucose. The breakdown of fat during fasting produces ketone bodies that can be used by neurons, but this alternate fuel only supplies about 60% of the brain’s energy needs because some neurons only operate on glucose. As a fallback measure, astrocytes in the brain minimize their own energy and oxygen needs to provide energy to the neurons when blood glucose levels are low. But if stress is increased this can lead to the death of astrocytes.
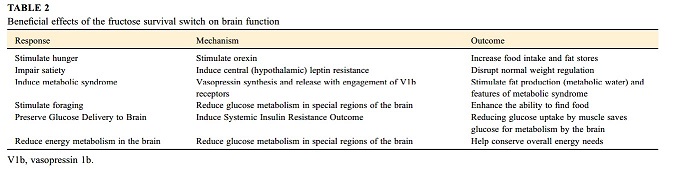
The fructose survival pathway helps the brain with the glucose it so desperately needs. It induces systemic insulin resistance to preferentially provide glucose to the brain.
It also stimulates a response that supports foraging, which costs energy, but is compensated for by reducing resting energy metabolism. Foraging requires focus, rapid assessment, impulsivity, exploratory behavior and risk taking. It is enhanced by blocking whatever gets in the way, like recent memories and attention to time. Fructose helps dampen these centers, allowing more focus on food gathering. The tendency for some Alzheimer’s patients to wander could possibly be left over from the ancient foraging response.
Early findings in Alzheimer’s research identified a reduction in glucose metabolism and intracellular ATP levels in certain regions of the brain: hippocampus, entorhinal cortex, posterior cingulate cortex, and middle temporal gyrus, while sparing other regions. This corresponds to the regions that fructose effects.
This reduced metabolism in certain regions of the brain was meant to temporary and reversible. But if the metabolism is chronically depressed as a result of continuous fructose metabolism, this leads to brain atrophy and neuronal loss, i.e. the features of Alzheimer’s disease.

Other food and conditions that stimulate fructose production

Foods that seem to put a person at greater risk of Alzheimer’s disease are also associated with fructose production or engagement of the fructose survival pathway. These include table sugar, high fructose corn syrup, high-glycemic carbohydrates, salty food and alcohol. Also processed meats rich umami or monosodium glutamate (described as the meaty, savory deliciousness, known as a fifth taste along with sweet, sour, bitter, and salty). Could Alzheimer’s disease be a maladaptation of an evolutionary survival pathway mediated by intracerebral fructose and uric acid metabolism?(Richard J. Johnson et al, Mar 2023)
Glucose
Note that fructose does not supplant glucose in importance. Glucose produces all the same features of obesity and metabolic syndrome as fructose, just via different means. Both are important, however, glucose loading also stimulates fructose production via the polyol pathway. About half the fat stored on the body comes from the glucose-insulin pathway and half from glucose-fructose conversion, so they’re both critical. Someone with high blood glucose levels (a diabetic) is making fructose all the time. A high carbohydrate diet also converts to fructose. But a low carbohydrate diet blocks the ability for the body to make fructose from glucose.

Salt
By increasing osmolality, salt can also stimulate fructose production. Ever wondered why deer like salt licks (sodium choloride)? It helping them put on weight for the winter. Salt stimulates the enzyme that converts glucose to fructose with salt. High salt intake causes leptin resistance and obesity in mice by stimulating endogenous fructose production and metabolism(Miguel A. Lanaspa et al, March 5, 2018)

Dehydration (and a salty diet)
Survival depends on having enough water. The body requires a lot of water to maintain an internal temperature balance and keep cells alive. In general, a person can survive for about three days without water. But fat, when it breaks down, can produce water. Many animals use fat not just for energy, but for water (think camel). Also, animals use that extra fat they accumulated from eating lots of fruit in the fall to use for water while hibernating.
There’s a hormone, called vasopressin, that we and animals produce when dehydrated. Vasopressin helps concentrate the water in the body by suppressing losing the water through the urinary tract, it also likely reduces water vapor loss through the lungs, and lowers body temperature to help reduce water loss.

Fructose also stimulates vasopressin. Likewise, when salt was given to animals, it stimulated vasopressin. It seems vasopressin drives fat because that is a survival mechanism to hold onto water.
Vasopressin is also high in obese people. In this study, Copeptin, a marker of vasopressin, in abdominal obesity, diabetes and microalbuminuria: the prospective Malmö Diet and Cancer Study cardiovascular cohort(S Enhörning et al, 22 May 2012) 2064 subjects were followed for 15 years, and they found a direct relationship of high vasopressin levels predicting obesity, diabetes, or metabolic syndrome years later.
To test this, researchers took animals and blocked different vasopressin receptors. When the V1B receptor was knocked out, the animals were protected from sugar, salt and from obesity. So vasopressin is a hormone that helps drive fat, driven by dehydration. Salt and even consuming sugar contributes to becoming dehydrated.
Studies have shown that obese people tend to: be high in serum sodium (salt), maintain a high sodium diet, do not drink a lot of water, and tend to be dehydrated. This is another reason to avoid processed and restaurant food in addition to added sugars, they also have high levels of salt.
So drink water! Water corrects dehydration and suppresses vasopressin, thereby suppressing the development of obesity and insulin resistance. Drinking 8 cups of water a day is a good recommendation. Urine should be light yellow, not clear or dark yellow.
Fructose

Fructose consumption may increase fructose production in the brain, possibly by raising uric acid. According to this paper Could Alzheimer’s disease be a maladaptation of an evolutionary survival pathway mediated by intracerebral fructose and uric acid metabolism?(Richard J. Johnson et al, Mar 2023)
- For example, acutely raising serum uric acid increases uric acid in both the hypothalamus [40] and the hippocampus [68, 69] in association with local inflammation. In turn, uric acid stimulates fructose production and metabolism [36, 70].
Traumatic Brain Injury (TBI)
Traumatic Brain injury results in inadequate blood supply (ischemia) localized to the area of injury. That decreases oxygen supply (hypoxia). In response, the brain increases localized fructose production.
Fructose and Alzheimer’s Disease
In early Alzheimer’s Disease, before the accumulation of the amyloid protein, three commonalities have been identified: Brain Insulin Resistance, Mitochondrial dysfunction/ATP depletion, and inflammation. That is exactly what fructose does.
Insert graphic Fructose vs AD. There are three commonalities between the effects of fructose in the body and early Alzheimer's Disease.
The brains of patients with Alzheimer’s Disease (AD) also hold greater levels of fructose. From Could Alzheimer’s disease be a maladaptation of an evolutionary survival pathway mediated by intracerebral fructose and uric acid metabolism?(Richard J. Johnson et al, Mar 2023):
- There is also evidence that fructose production and metabolism are increased in the brains of patients with AD, especially early in the disease before marked neuron loss and atrophy. One study used mass spectrometry to measure components of the polyol pathway in postmortem regions of the brains of 9 subjects with AD and 9 age-matched controls. Sorbitol and fructose levels (both components of the polyol pathway) were significantly elevated, averaging 3–5-fold higher in all regions of the brain studied, including the hippocampus, entorhinal cortex, middle temporal gyrus, cingulate cortex, sensory and motor cortex, and cerebellum (Figure 3) [96]. One control subject also had high levels of fructose and sorbitol but had no premortem evidence of dementia; however, the patient had preclinical AD, as noted by low brain weight and Braak stage II histopathologic changes [96].
Does fructose effect ApoE4s more?
For the vast majority (approximately 96%) of human history, we were all ApoE4 homozygotes (ε4/4). The double allele aided early man to survive under very challenging conditions inciting inflammation, parasites, periods of food paucity, and more. But the ApoE4 allele is decreasing in number and seems ill-adapted to modern times.
Similarly, the biochemical responses that fructose induces in humans and other animal bodies have aided survival during difficult times. But for humans in modern times, fructose induces deleterious health effects.
From Could Alzheimer’s disease be a maladaptation of an evolutionary survival pathway mediated by intracerebral fructose and uric acid metabolism?(Richard J. Johnson et al, Mar 2023):
- Apolipoprotein E4 (ApoE4) polymorphism is a major risk factor for AD, raising the question of how it relates to the fructose hypothesis. Notably, ApoE4 carriers show reduced cerebral glucose metabolism by positron emission testing and reduced uptake of glucose into astrocytes [143]. ApoE4-derived astrocytes also show enhanced glycolysis despite less mitochondrial OXPHOS and worse mitochondrial dysfunction compared with that with ApoE2 or ApoE3 astrocytes [143]. The relative similarities in the effects of fructose on the brain to that observed with the ApoE4 polymorphism suggest parallel pathogenic mechanisms.
In other words, ApoE4 susceptibilities relate to directly to fructose’s effect on the brain, suggesting ApoE4s are at greater vulnerability to the effects of fructose and might explain our greater risk for sporadic Alzheimer's Disease.
This is still a hypothesis
While the similarities between fructose and Alzheimer's are compelling, the science is not settled and there are some issues that need to be better understood. Further studies are needed. Also, tThe intricacies of this hypothesis are also far more involved than what has been represented here, this wiki endeavored to provide the most salient points of this hypothesis.
About the lead researcher, Richard J. Johnson
Richard J. Johnson is a physician and scientist whose primary interest has been on the causes of obesity and diabetes. He is a Professor of Medicine at the University of Colorado.
Dr Johnson’s specialization is nephrology. Nephrology is known as the thinking man’s specialty. The field attracts individuals who prefer logic and deductive reasoning. Nephrologists need to think systemically since many diseases that affect the kidney are rarely limited to the just organ itself.
Much of Dr Johnson’s work, supported by the National Institutes of Health, has focused on sugar and especially on fructose, as well as one of the products of fructose metabolism, uric acid.
Dr Johnson has published numerous papers (>500) and has lectured in over 40 countries. Recently he has published a book, Nature Wants Us to Be Fat, that discusses much of his work and discoveries.
He has a webpage https://drrichardjohnson.com/ which provides links to his research publications, videos, podcasts, and additional resources for further pursuit on his research.